Intracavernosal injection therapy for erectile dysfunction
The management of patients with erectile dysfunction has recently been grouped into three different levels. Initially, patients should be advised to control every clinical abnormality or life-style factor associated with a higher risk of erectile dysfunction. 
Usually, this first step alone is not able to cause a significant improvement of the patient’s erectile function, and first-line therapy is considered. This includes oral pharmacotherapy, use of a vacuum device or psychosexual therapy. The majority of patients who are currently seen for erectile dysfunction are prescribed either sildenafil or
apomorphine sublingual, the two drugs that are officially marketed.
This happens because the efficacy and safety of the oral approach have been clearly established, and because most patients would rather undertake a therapy that is simple to use. Patients who do not respond to oral therapy are considered for second-line treatment, which includes intraurethral or intra-cavernosal administration of vasoactive drugs. To date, it has been rare to prescribe one of the second-line therapies when choosing treatment for the first time: this used to happen when sildenafil was the only oral drug on the market, as patients using nitrates had a definite contraindication to the use of sildenafil.
A second patient category might be represented by those requesting a fast response that could not be obtained with sildenafil; however, apomorphine sublingual is characterized by a fast on set of action, and may represent an effective solution for these patients. In conclusion, intraurethral and intracavernosal therapies are currently used almost exclusively in patients who fail to respond to oral therapy; however, when counselling the patient with
erectile dysfunction on the treatment options available, every alternative should be extensively detailed at the first office visit.
The aim of this article is to review the latest results obtained with these therapeutic options, and to demonstrate the correct approach to patients candidate for these therapies.
Intracavernosal injection therapy
When a patient is considered a potential candidate for vasoactive injection therapy, the characteristics of the treatment are extensively explained along with the potential limitations and adverse effects. He is asked to read and sign a detailed informed consent. 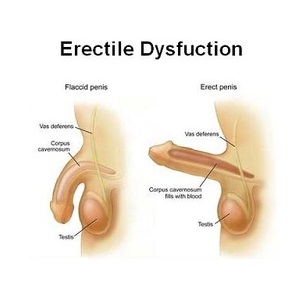
Patients with a history of hemoglobinopathy, bleeding diathesis, Peyronie’s disease or idiopathic priapism are excluded from treatment. In addition, patients with poor manual dexterity, poor visual acuity or morbid obesity, or those in whom a transient hypotensive episode may have a deleterious effect (e.g. unstable cardiovascular disease and transient ischemic attack), are not ideal candidates for this treatment. Finally, patients with serious
psychiatric disorders or patients who might misuse or abuse this therapy should be excluded from treatment.
The first phase of the pharmacological erection program consists of dose titration of the drug or mixture used for injections. Patients are placed in the sitting position on the examination couch during each injection and kept in this position for 30 min. Systemic blood pressure is recorded as baseline in the event of syncope, and to check for
hypertension. The right side (lateral aspect) of the penis is cleansed with an alcohol swab.
The first injection is then performed with a very small amount of either the drug or the mixture. The needle is inserted by a quickjab up to the hilt of the needle so that the tip of it reaches the centre of the right corpus cavernosum. Injections must not be performed on the dorsal and ventral aspect of the penis, to avoid damage to the dorsal neurovascular bundle of the penis and the urethra, respectively.
Immediately after injection, the base of the penis is squeezed firmly between the right thumb and index finger, while the accessible portion of the penis is massaged for up to 5 min by squeezing it laterally along the length of the shaft between the left thumb, and index and middle fingers, thus distributing the drug throughout the pendulous shaft. Patients are then left alone to watch an erotic video and they are invited to masturbate without ejaculation to optimize sexual stimulation. The erectile response is then assessed by the physician and the patient. The dose of the injected drug or mixture is considered adequate when it produces an erection equal to 50–75% of the maximal erectile response reported by the patient.
If a patient reaches a maximal rigid erection during the titration phase in the clinic, a lower dose is suggested for home use as the erectile effect induced by the drug or mixture during sexual activity is usually greater than that observed under laboratory conditions. If the first injection does not produce a satisfactory erectile response (that is, less than 50% of the maximal potential response), the patient is re-injected after at least 24 h and the dose is slightly increased. The titration process proceeds until the optimal dose is identified or the maximal injected volume is reached.
At our clinic, three versions of a four-drug mixture composed of papaverine, phentolamine, alprostadil and atropine sulfate are used, and 0.05 ml is usually injected first. We subsequently use 0.05-ml increments. If after the injection a fullrigid erection persists for longer than 1 h, 20–40 μg of adrenaline is injected intracorporeally to obtain complete detumescence. Appropriate electrocardiographic and blood pressure monitoring are used during this procedure.
Patients are contacted by telephone the next day to verify persistence of detumescence. After the appropriate dose of the drug or mixture has been determined, patients watch the thorough demonstration of both a conventional insulin syringe and an automatic selfinjection system (Disetronic pen®; Medis, Milan, Italy) with which multiple injections can be performed, thus avoiding the maneuvers needed before each injection performed with the insulin syringe (preparation of the syringe, needle and appropriate amount of the drug). The pen consists of a capsule that is screwed together with the adaptor after inserting the filled glass cartridge. The needle is then screwed into the
adaptor.
The glass cartridge consists of a rubber piston and a conus in front, which is closed with a cap. The cartridge set contains a pull rod and a needle in addition to the glass cartridge. To fill the cartridge, the pull rod is screwed into the thread of the rubber piston and, after removing the cap, the needle is stuck upon the conus. The glass cartridge volume is 3 ml. At our clinic the cartridge is filled with a four-drug vasoactive mixture, which is described in detail below. Astheaverage volume of mixture used at each injection by our patients is below 0.2 ml, every cartridge has a drug load that is usually enough for 8–10 injections. We supply 29-gauge needles for injections.
To prepare the pen for injection, the adaptor is first removed from the capsule. The full glass cartridge is then inserted into the capsule with the conus pointing forward. The adaptor is screwed firmly into the capsule. The needle is removed from the blister and screwed together with the cap into the adaptor. The needle cap is pulled out and, while the pen with the needle is held pointing upwards, the knob is pressed slowly until it reaches the top.
Some drops of liquid should come out, but if this does not occur the knob is turned clockwise for approximately 2–3 clicks and is slowly pressed until it stops. The knob is slowly released, drops are shaken off and the cap is put into the adaptor. To inject the drug, the needle is inserted into the corpus cavernosum and the pen knob is gently
depressed until it stops. Two models of this system are currently available, which differ only in the volume (20 or 50 μl) of liquid released with every click of the knob. We currently use 20 μl for pure psychogenic and neurogenic patients, and 50 μl for vasculogenic cases.
Patients are instructed to limit injection use to three times a week, with no more than one injection in any 24-h period. They are also taught to inject the right and left cavernous body alternately. Patients are then warned to return immediately to the emergency room if erection persists for longer than 3 h. Patients are also told to
refrigerate the drug or mixture, if it contains prostaglandin E1, and to examine the drug or solution for changes in color or the formation of a precipitate.
Patients are reassessed once a month for the first 2 months, and subsequently every 3 months. At each follow-up visit, injection frequency, duration and consistency of erections, and patient satisfaction are recorded. The penis is carefully examined for nodules, hematomas or areas of induration. Liver function is assessed every 6 months.
Penile ultrasonography is performed to verify any clinical findings on digital palpation of the penis.






